Prostate cancer: warning signs, diagnosis and treatment
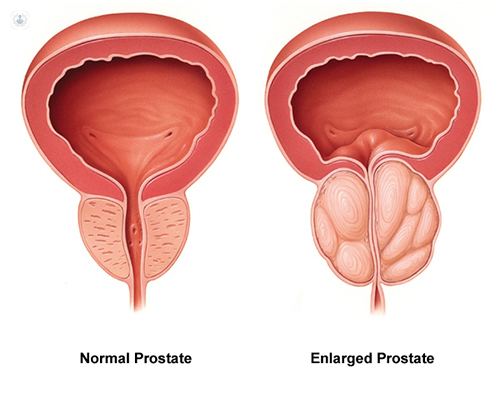
Written by:The prostate is an organ that is unique to men rather than women. Men are born with a prostate gland that is small and as one gets older, the prostate gland gets bigger. As it gets bigger, it can restrict your urinary flow and that can cause problems in men as they get older. It can also be the site or development of a prostate cancer which requires treatment in men as they get older. Mr Rick Popert, expert urologist, discusses the most important warning signs for prostate cancer, and how it is diagnosed and treated.
What are the main warning signs & symptoms to be aware of for prostate cancer?
The first issue with the prostate gland is that because it gets bigger, it may restrict the urinary flow between the bladder and the urethra so men may complain of hesitancy, poor flow and incomplete emptying. These are usually signs of prostate enlargement and in people who have got an enlarged prostate with a significant cancer, this may be how they present their symptoms.
However, most men will present with no symptoms. They may simply have an elevated PSA blood test. This blood test stands for prostate specific antigen and is prostate specific, it is not prostate cancer specific. However, a PSA level can give an indication that somebody is at risk of developing prostate cancer. We usually recommend that this is tested from the age of 50 or from the age of 40 in men who have a family history of prostate cancer. It is also important to know what your own baseline PSA is. If the PSA in the 40-year-old man is above 2, that could certainly be suspicious for early prostate cancer; above 3 in a 50-year-old man and above 4 in a 60-year-old man.
How is prostate cancer diagnosed?
Men may present signs of prostate cancer because they have urinary symptoms or because they have the elevated PSA blood test. We can sometimes identify prostate cancer on a physical examination of the prostate which is done through the back passage with a finger. However, that is not the most accurate way to diagnose prostate cancer.
The most modern technique is to use an MRI scan of the prostate which allows us to visualise the shape of the prostate and identify if there is any area within the prostate gland that we might say does not look right and looks like it may be a cancer. In those situations we can then do prostate biopsies in which we take some samples from the prostate to see if we can find the cancer visualised by the MRI scan or if the MRI scan is normal. However, if the PSA blood test remains elevated, we may still want to do biopsies around the prostate gland. The important thing to understand is that the prostate gland can harbour prostate cancer silently and therefore biopsies are necessary to identify whether there is any cancer in the prostate.
How is prostate cancer treated?
Once a prostate cancer diagnosis has been made, we have some information from the biopsy that gives us an idea about the grade of the cancer. That tells us something about how potentially aggressive it may be. Some prostate cancers are low grade, non-aggressive and they may grow very, very slowly for many, many years and they may require no treatment. In that situation, we will monitor the PSA over time and that is called active surveillance.
In patients who have a higher grade of tumour, we may offer them either some form of radiotherapy treatment or some form of surgery. The radiotherapy treatments lie between brachytherapy where we put radioactive seeds individually into the prostate to kill a prostate cancer in situ or external beam radiotherapy where the radiation is beamed in from outside the body.
Read more: Brachytherapy for prostate cancer
In both of these treatments, the prostate gland remains in place in the body. Surgery, however, requires removal of the prostate gland. From 10 years ago, this surgery was routinely done by open surgery. Nowadays, we can actually do the surgery less invasively using keyhole surgery and robotics. This allows us to remove the prostate gland much more safely with less morbidity, particularly with regards to urinary incontinence or erectile dysfunction.
What is the outlook for people with prostate cancer?
Although prostate cancer is the commonest form of malignancy in men, most men will not die from prostate cancer. If it can be caught early and adequately treated, most people will have a normal life expectancy. The critical thing with diagnosing and treating prostate cancer is to identify significant disease early and to offer an appropriate treatment early so that the long-term effects of prostate cancer spreading outside the prostate gland itself are avoided. In that way, most patients will have a normal life expectancy.
If you would like an expert's opinion, make an appointment with a specialist.


