Understanding bronchiectasis
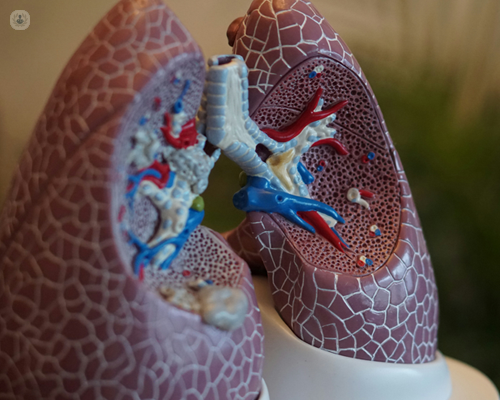
Written by:Bronchiectasis is a chronic respiratory condition characterised by abnormal widening and thickening of the airways (bronchi), which can result in recurrent or persistent chest infections and chronic inflammation of the airways.
Leading respiratory medicine specialist Dr Dean Creer provides simple and informative answers to key questions about bronchiectasis for adults who may be affected by this condition.
What causes bronchiectasis?
Bronchiectasis can develop due to various factors, including:
- Infections: Severe or recurrent respiratory infections in childhood or in adults, such as pneumonia or tuberculosis, can cause permanent damage to the airways resulting in bronchiectasis.
- Autoimmune conditions: Certain autoimmune diseases, such as rheumatoid arthritis or inflammatory bowel disease, may increase the risk of bronchiectasis.
- Genetic factors: In some cases, bronchiectasis can be inherited due to conditions like cystic fibrosis or primary ciliary dyskinesia although this is much less common in adults than in children.
What are the symptoms of bronchiectasis?
Common symptoms of bronchiectasis include:
- Chronic cough: Persistent cough that may produce large amounts of mucus (sputum) from the chest.
- Frequent chest infections: Recurrent chest infections leading to increased production of sputum.
- Fatigue: Feeling tired or lethargic due to the body's efforts to fight infection and maintain normal lung function.
- Shortness of breath: Difficulty breathing, especially during physical activity.
How is bronchiectasis diagnosed?
Bronchiectasis is typically diagnosed through a combination of:
- Medical history: Discussing symptoms, past respiratory infections, obtaining a history of underlying health conditions and taking a family history.
- Physical examination: Including listening to the lungs with a stethoscope for abnormal sounds.
- Imaging studies: Chest X-rays are usually performed as initial imaging the chest, however the gold standard is a high resolution CT scan of the chest (HR CT CHEST) to visualise the airways and identify any other abnormalities including looking for characteristic features of different types of infections.
- Sputum cultures: Sputum samples (mucus) are requested to identify any bacteria or other pathogens causing infection.
- Blood tests: Blood tests are often performed to help characterise the cause of bronchiectasis and to assess for possible complications of bronchiectasis.
- Breathing tests Breathing tests are periodically performed to assess the severity of bronchiectasis.
What are the treatment options for bronchiectasis?
Treatment for bronchiectasis aims to:
Clear airways
Seeing a chest physiotherapist to learn effective airway clearance techniques help remove excess mucus (sputum) from the lungs.
Manage infections
Antibiotics (most commonly for an extended period of 10-14 days) are usually prescribed to treat bacterial chest infections and can be prescribed for prolonged periods in selected patients to prevent exacerbations (flare-ups).
Control symptoms
Inhaled bronchodilators may help relieve shortness of breath and wheezing.
Medications to help loosen the sputum (mucus) and help to clear the sputum (expectorate) are called mucolytics which can also help prevent and treat infections.
Can progression of bronchiectasis be prevented?
- Vaccinations: Staying up-to-date on vaccinations, including flu and pneumonia vaccines, can help prevent respiratory infections.
- Smoking cessation: Quitting smoking reduces the risk of recurrent infections and of developing other chronic lung diseases like COPD.
- Prompt treatment of respiratory infections: Seeking prompt medical attention for respiratory infections helps prevent complications and reduce the risk of lung damage.
What is the prognosis for bronchiectasis?
The prognosis for bronchiectasis varies depending on factors such as the underlying cause, the severity of the condition, and how well it responds to treatment. With appropriate management, many, if not most, individuals with bronchiectasis can lead fulfilling lives and maintain good respiratory health.
Are there complications associated with bronchiectasis?
Yes, undiagnosed, untreated or poorly managed bronchiectasis can lead to complications such as:
Chronic respiratory infections
There are specific infections with bacterial, fungal or mycobacterial organisms that can cause chronic infection leading to further damage to the airways and lungs.
Respiratory failure
Severe lung damage can impair lung function, leading to respiratory failure.
Pulmonary hypertension
Increased pressure in the blood vessels of the lungs can strain the right side of the heart and lead to pulmonary hypertension.
Bronchiectasis is a chronic respiratory condition that requires ongoing management to maintain lung health and quality of life. Understanding the causes, symptoms, treatment options, and preventive measures can empower individuals to take control of their respiratory health and work closely with healthcare providers to manage bronchiectasis effectively.
If you experience symptoms suggestive of bronchiectasis, seek medical attention for evaluation and appropriate management. Early diagnosis and treatment can help minimise complications and improve long-term outcomes for individuals living with bronchiectasis.
If you require expert bronchiectasis treatment, arrange a consultation with Dr Creer via his Top Doctors profile.


