Sperm retrieval
What is sperm retrieval?
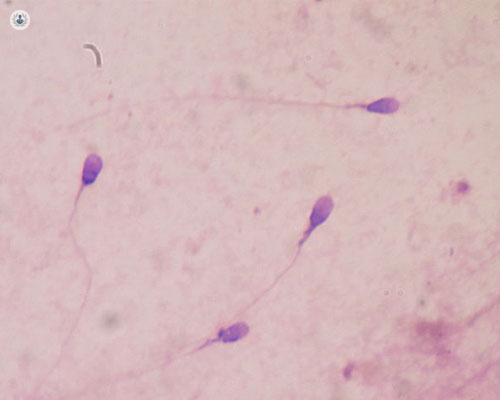
Sperm retrieval is the surgical extraction of sperm from the testicles in the case that a has obstructive azoospermia (a blockage is preventing healthy sperm from being ejaculated) nonobstructive azoospermia (the body produces too few sperm or isn’t producing any).
A lack of sperm can be due to:
- An obstruction that prevents sperm from being released, potentially caused by injury or infection
- Having had a vasectomy
- Non-obstructive azoospermia (when the testicles don’t produce enough sperm)
- An absence of the vas deferens at birth – the vas deferens is the tube that drains the sperm from the testicle
Why is it done?
Sperm retrieval is used when a couple wishes to conceive but aren’t able to do so naturally. It’s used for men who can’t ejaculate or who have little or no sperm in their semen and decide to participate in IVF (in vitro fertilisation) treatment.
What does sperm retrieval involve?
There are several sperm retrieval methods and the collection of sperm is generally coordinated with egg retrieval from their female partner. The procedures are:
- Percutaneous Epididymal Sperm Aspiration (PESA) : Sperm is extracted directly from the epididymis (which transports and stores sperm from the testes) via a fine needle.
- Microepididymal Sperm Aspiration (MESA): Sperm is collected directly from the epididymal tube using a microscope.
- Testicular Sperm Aspiration (TESA)/ - also referred to as testicular fine needle aspiration (TEFNA) : Using a needle attached to a syringe, fluid containing sperm is sucked out from inside the testicles.
- Testicular sperm extraction (TESE): Sperm is collected via a biopsy (or multiple biopsies) of testicular tissue. In involves an incision into the scrotum.
- Microsurgical Testicular Sperm Extraction (microTESE): Similarly to the TESE, sperm is collected via a biopsy (or multiple biopsies). However, a microscope is used to identify the tissue with the highest likelihood of containing suitable sperm.
Your specialist will guide you on the pros and cons of each procedure.
What is recovery time like?
With procedures such as TESA (testicular sperm aspiration), recovery is shorter and less painful than testicular surgery in which an incision is made, which might require a recovery of almost seven days. There might be soreness as a side effect and as with any surgical treatment, infection is a risk. You may be asked to avoid physical activity and depending on if you have pain, be provided with pain medication.
What are the alternatives to sperm retrieval?
If a man does not wish to undergo a procedure to retrieve sperm but wishes to have a child, they may consider using trying to conceive naturally, to adopt, or to use donor sperm.




