Cardiac resynchronisation therapy
Professor Mark Gallagher - Cardiology
Created on: 07-21-2014
Updated on: 05-24-2023
Edited by: Conor Lynch
What is cardiac resynchronisation (CRT) therapy?
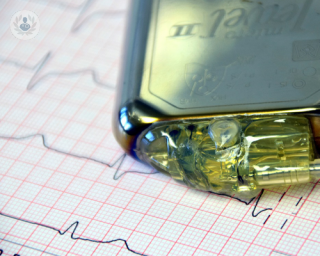
Cardiac resynchronisation therapy is a treatment used to help the heartbeat achieve the right rhythm. Cardiac resynchronisation therapy uses a pacemaker to restore the normal rhythm of the heartbeat.
The pacemaker coordinates the timing of the upper heart chambers and the lower heart chambers. It also improves the timing between the right and left sides of the heart.

When your heart doesn't pump strong enough, fluid can build up in your legs and lungs. This is known as heart failure. This condition can occur when the two bottom chambers of the heart (ventricles) won't beat at the same time.
Your doctor may discover that an implantable cardioverter-defibrillator (ICD) is also needed. It's a device that helps to fix serious heart rhythm issues. If this device is needed, it may be combined with CRT.
Why is cardiac resynchronisation therapy done?
CRT may be suggested by your doctor for the following reasons:
- You have severe or moderate symptoms of heart failure.
- The pumping chambers of your heart are not working together.
- Tests show that your heart is enlarged and weak.
- Lifestyle changes and medications are not working well enough to control your heart failure.
What does CRT consist of or involve?
CRT involves getting an implantable cardioverter-defibrillator by having minor surgery. Wires from the device are attached to the ventricles of your heart. The CRT device sends electrical signals to these areas to make the heart pump properly.
CRT usually works treating most cases of heart failure. However, not everyone with heart failure can be helped by CRT. For example, if you have advanced heart failure, you are not as likely to respond to CRT.
Overall, CRT may improve your survival, quality of life, and heart function, if you have mild to moderate heart failure. It also improves your ability to exercise.
After surgery, you'd be moved to the recovery area. You would stay there until the relaxing medicine has worn off. Pain medicines are likely to be needed.
Patients may have to stay in the hospital for a day or two whilst the doctor checks and adjusts settings on your new CRT device.
After the patient leaves the hospital, it will be important to follow the doctor's advice and attend follow-up appointments.
What aftercare should be carried out?
- Normal diet can be resumed.
- Activities such as straining, lifting and stretching for the first six weeks are limited.
- The dressing should remain clean until the doctor says it's ok to remove the dressing.
- The incision area should be checked for any signs of infection. The doctor hould be notified if there is redness, fever, soreness, bleeding, discharge, or swelling.
The long-term instructions for living with your CRT device usually mean:
- Ensuring your doctor checks the functioning of your device regularly.
- That your pacemaker battery will last for about four to eight years. It's important to monitor it and replace the CRT pacemaker when needed.
- You might need to stay away from electronic devices that have strong magnetic fields. These include appliances like microwaves and electrical generators. You should speak to your doctor if you have any questions about what to avoid.
How do you prepare for cardiac resynchronisation therapy?
Risks and benefits of CRT should be discussed with your doctor. They will probably tell you to not eat or drink anything after midnight before surgery. If you usually take medicines when you wake up in the morning, ask your doctor if you can still take them.
Patients may be asked to stop taking medication that thins blood several days before the procedure. Those who take medication for diabetes should ask doctors for help in order to adjust the dosage around your surgery.
Let your doctor know about:
- Prescription drugs that you take
- Over-the-counter medicines or supplements you take.
- Allergies
- Recent symptoms of infections or colds.
- History of problems with anaesthesia.