Osteoporosis
Professor Gordana Prelevic - Endocrinology, diabetes & metabolism
Created on: 04-22-2013
Updated on: 05-02-2023
Edited by: Conor Dunworth
What is osteoporosis?
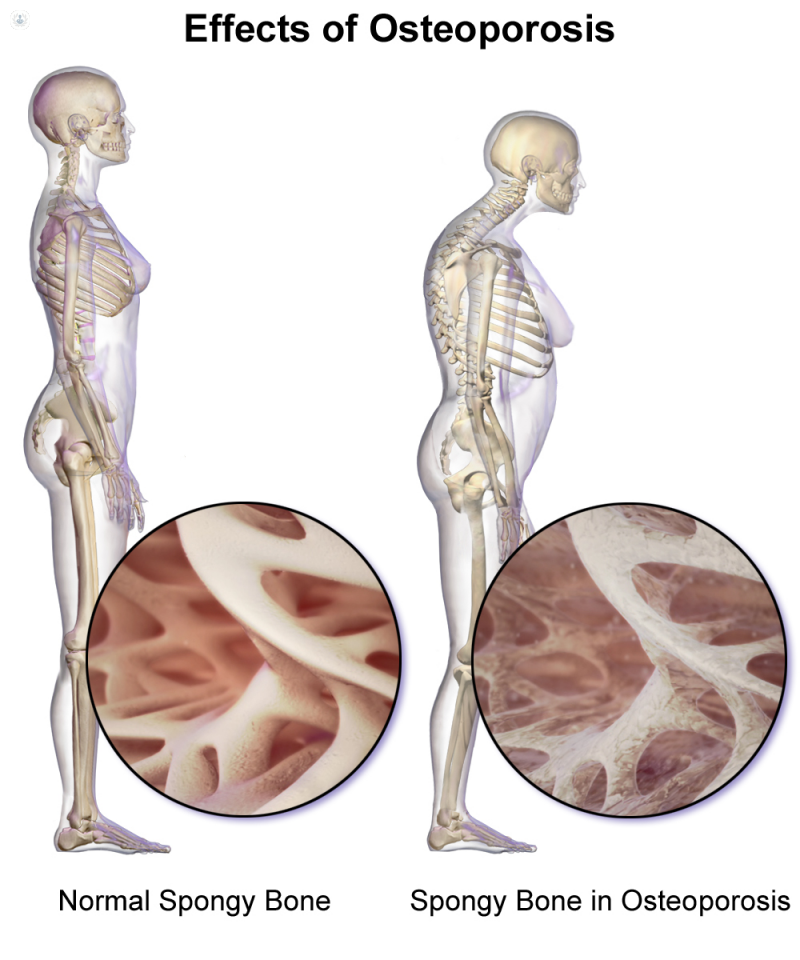
Osteoporosis, meaning “porous bone”, is a condition in which the bones become weak and brittle, due to the body either losing too much bone or making too little.
On a microscopic level, the structure of healthy bones resembles a honeycomb, with hollows and spaces. In bones affected by osteoporosis, these hollows and spaces are much wider, meaning the bones are less dense and therefore weaker than they should be. This makes them susceptible to breaks (fractures).
What are the symptoms of osteoporosis?
Osteoporosis is a “silent” disease without any symptoms. Most of the time, a person will not realise they have osteoporosis until they break a bone. Osteoporosis fractures also called fragility fractures (caused by minor trauma) occur most commonly at the wrist, spine and hip.
Breaks can also occur in the arms or pelvis and sometimes, in severe osteoporosis, a sneeze or a cough will lead to a broken rib or the partial collapse of a spinal bone.
Stooped posture (in older people) and particularly significant loss of height (>2 inches) should always prompt investigation for osteoporosis.
Over 500,000 people in the UK receive treatment for fragility fractures every year due to osteoporosis. Fragility fractures are fractures that occur with minor trauma (like falling from standing height or less which normally would not cause a fracture in a person without osteoporosis.
What are the medical tests to diagnose osteoporosis?
The DEXA or DXA scan is a reliable method to measure bone mineral density (BMD) using a low-intensity X-ray. It is painless, straightforward (taking 10 to 20 minutes), and involves minimal radiation – in fact, the operator sits in the same room as the patient.
After the scan is done, the results are compared to that of a young, healthy individual, and based on accepted criteria a diagnosis of osteoporosis may be made. The difference is called a T- score: a T- score of above -1 is normal, while a T- score below -2.5 is consistent with the diagnosis of osteoporosis.
The 10-year probability of breaking a bone could be calculated using a FRAX calculation tool which takes into consideration hip neck bone mineral density and various other clinical risk factors.
What are the causes of osteoporosis?
Losing bone is a natural part of getting older, but some people will lose bone density faster than others. In general, women have a higher risk of getting osteoporosis than men, especially in the years following the onset of the menopause, when bone density is lost more rapidly. This is especially the case for women who have had their ovaries removed or if menopause has begun early (before the age of 45).
Factors that can increase the risk of osteoporosis include:
- A family history of osteoporosis
- Certain medical conditions, e.g., inflammatory bowel disease, malabsorption problems, Coeliac disease, thyrotoxicosis, hyperparathyroidism, rheumatoid arthritis, multiple myeloma etc.
- Certain medications: corticosteroids, heparin, excessive thyroxine, Depo-Provera, and some cancer drugs (anti-oestrogens in particular).
- Heavy drinking and/or smoking
- Low body weight and anorexia nervosa
Can osteoporosis be prevented?
While it is impossible to prevent a condition like osteoporosis with 100 per cent certainty, you can lower the risk of getting the disease by taking steps in your lifestyle to keep your bones healthy:
- Regular exercise, such as any moderate-intensity activity, weight-bearing exercise and resistance exercise
- Calcium-rich diet and vitamin D supplementation
- Giving up smoking and reducing alcohol intake
What is the treatment for osteoporosis?
Treating osteoporosis revolves around treating fractures caused by the condition and trying to improve bone strength, which may involve medication. Your doctor will advise you on starting treatment depending on the T-score results of your DXA scan and your future fracture risk.
Most of the therapies available slow down the rate of bone loss and decrease fracture risk except for parathyroid hormone analogues which effectively stimulate bone formation.
Possible treatments include:
- Bisphosphonates which slow the rate of bone loss. They could be in the form of tablets (alendronic acid, risedronate, and ibandronate) or injections (zoledronic acid).
- Hormone replacement therapy (HRT) – sometimes recommended for menopausal women, as it can control menopausal symptoms and also help maintain the strength of the bones. However, HRT is rarely used only for treating osteoporosis in the absence of menopausal symptoms.
- Testosterone treatment – if osteoporosis is a result of hypogonadism (low production of male sex hormones) in men.
- Raloxifene is a Selective oestrogen receptor modulator (SERM). It maintains bone mineral density and lowers the risk of fracture.
- Denosumab (Prolia) – subcutaneous injections at six monthly intervals
- Parathyroid hormone analogues – delivered via daily subcutaneous injection can actually increase bone density by stimulating the cells that create new bone.
Which type of specialist treats osteoporosis?
Endocrinologists and rheumatologists treat osteoporosis.
Are osteoporosis and osteoarthritis the same?
While people can have osteoporosis and osteoarthritis at the same time, osteoarthritis is a degenerative joint disease caused by injuries or everyday wear and tear, which leads to the loss of the cartilage between the bones. Osteoporosis, on the other hand, is the loss of bone mass, which increases the risk of bone fractures. Both conditions are prevalent in the elderly population.
Are osteoporosis and scoliosis related?
Although osteoporosis and scoliosis both affect the spine, scoliosis is a sideways curvature of the spine that mostly affects younger patients. It is also possible for a person to have scoliosis and osteoporosis at the same time.
An elderly person with osteoporosis can end up developing scoliosis as well, because osteoporosis can cause bones in the spine to weaken to the point of crumpling. This leads to loss of height and a curved spine.
Are osteoporosis and osteopenia the same?
Osteopenia is the stage of bone loss before osteoporosis: when your bone density is lower than the average for your age, but not low enough to be classified as osteoporosis.
Can osteoporosis be reversed?
While osteoporosis is a chronic condition that cannot be completely reversed, treatment and lifestyle changes can help to prevent further bone loss, sometimes improve bone mineral density and most important prevent fragility fractures.
















