Parathyroid gland surgery
Miss Aimee Di Marco - Surgery
Created on: 03-16-2017
Updated on: 10-05-2023
Edited by: Karolyn Judge
What is parathyroid gland surgery?
Parathyroid gland surgery seeks to remove one, various, or all of the parathyroid glands in order to treat overactive parathyroid glands. If the parathyroid is abnormal, it can cause various medical complications. In such cases, parathyroid gland surgery, otherwise known as parathyroidectomy when glands are removed, may be necessary.
Why is parathyroid gland surgery performed?
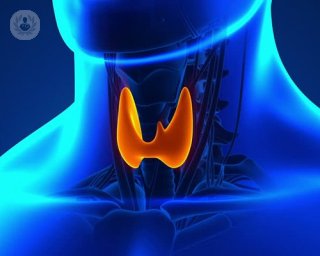
The parathyroid glands are in fact four individual glands found on the thyroid, which is located in the neck. The parathyroid glands regulate calcium in the blood. If they detect that calcium levels are low, they release parathyroid hormone, taking calcium from the bones. If the parathyroid gland is abnormal, it can produce too much calcium, which leads to a condition called hypercalcaemia. This can have serious consequences, including kidney failure, hypertension, and coronary artery disease.
Parathyroid gland surgery may also be necessary in the following cases:
- If cancerous tumours are found on or near the glands
- If non-cancerous tumours, called adenomas, are found
- In those with a history of thyroidectomy, meaning the thyroid has been removed
- In parathyroid hyperplasia, where all parathyroid glands are enlarged
What does it involve?
The most common surgical approach is to make an incision in the neck, enabling the identified parathyroid gland to be removed. The traditional technique for removing parathyroid glands was a technique called bilateral neck exploration, in which the surgeon identifies exactly which of the glands requires removal. However, as many only need one gland removed, surgery these days attempts to be less invasive, meaning there is less scarring and less recovery time is needed.
Different techniques include:
- Focused parathyroidectomy, in which the neck is not explored, and one particular gland is removed after pre-operative tests.
- Video-assisted parathyroidectomy, where the surgeon cuts a small incision and inserts a small camera, which allows them to explore inside the neck more easily and guides them to the correct gland.
- Radio-guided parathyroidectomy, in which the surgeon uses a particular type of radioactive material that only the affected parathyroid glands will absorb, guiding them to the correct gland.
The type of surgery offered will depend on the patient and how suitable they are - there are various types of procedure and the surgeon will advise which is best. For example, in some patients, robotic-assisted surgery is now an option, in which an incision is made in the armpit rather than the neck. However, this is not always suitable and other techniques may be more fitting for the patient.
How can you prepare for parathyroid gland surgery?
An initial consultation must be made before the surgery is scheduled, to check if the patient is a candidate for parathyroid gland surgery. The surgeon will advise any precautions which need to be taken, and will explain what is safe to take regarding medications, if the patient has any prescribed. Blood thinners must not be taken for several days before surgery (e.g ibuprofen, aspirin).
As the procedure these days is most commonly minimally-invasive, it is often performed as a day case. However, in those who undergo traditional operations, an overnight stay is expected. In either case, transport to and from the hospital with a friend or companion should be arranged.
What's involved in post-operative care?
Parathyroid gland surgery is most commonly performed as an outpatient procedure, and patients are usually sent home the same day. After the operation, the patient should expect some discomfort - often described as similar to a sore throat. Patients will be able to swallow, but softer foods are often easier for the patient to deal with immediately after surgery. Over-the-counter painkillers can help with discomfort and pain.
After the surgery, a few days off work is expected, and driving should not be considered until the patient can turn their head from side to side, and is no longer taking medication for pain relief. The patient should expect a scar to form, which over the months following the operation will gradually fade until it is barely noticeable.