Thyroid gland surgery
Professor Neil Tolley - Otolaryngology / ENT
Created on: 11-13-2012
Updated on: 09-12-2023
Edited by: Conor Dunworth
What is thyroid gland surgery?
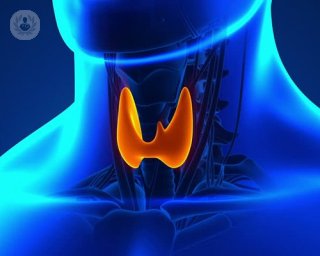
Thyroidectomy is the primary treatment for a number of thyroid problems. The thyroid gland sits in the neck and secretes hormones that regulate the body’s metabolism. For conditions that affect the gland, thyroidectomy is often the first-line treatment where all or part of the thyroid may be removed.

Why would you do it?
Thyroid problems are common. There are a number of conditions that can arise within the gland and many endocrine abnormalities are treated with medication. In some circumstances however, thyroidectomy is recommended to treat a range of conditions that affect the gland, including cancer, Graves' disease, recurrent cysts, or goitres (an enlarged thyroid gland) that are problematic.
What does it involve?
The procedure usually involves removing all or a portion of the thyroid. A total thyroidectomy would involve removing the whole gland, whilst a lobectomy removes half. Sometimes an isthmusectomy is performed to remove only the central part of the gland.
The portion of the thyroid that is to be removed will depend on the nature and extent of the condition.
There are three main types of surgery. Conventional surgery involves making an incision in the neck through which all or the required portion of the thyroid is removed. Endoscopic thyroid surgery involves the use of an endoscope inserted through a small incision in the neck.
Recently robotic thyroidectomy has evolved permitting the operation to be performed through incisions in the chest, armpit or even through the mouth.
In all cases, thyroid gland surgery is usually undertaken with a general anaesthetic.
How to prepare for it
As with any operation, a patient will be assessed for their suitability beforehand. Patients may also be required to fast for a period of 6 hours before surgery. When surgery is undertaken for the overactive gland Potassium Iodide or Lugol’s Iodine may also be started 5-10 days before surgery.
Post-operative care
In most cases, it is possible to leave the hospital after an overnight stay although hemithyroidectomy can occasionally be done as a day case. It is important to avoid putting strain on the neck for a week after the operation.
Neck pain and voice problems are not uncommon but usually resolve by themselves. In the case of a total thyroidectomy, where the whole thyroid gland is removed, the patient will need to take medication to compensate for the hormone usually produced by the gland itself. Post-operative calcium will also need to be monitored and temporary hypoparathyroidism can occur after a total procedure.
For a partial thyroidectomy, the remaining portion of the thyroid will often compensate for the entire gland in 70% of patients avoiding a need for thyroxine. Patients after thyroid surgery require an annual thyroid function test for life.