What should I expect from an ERCP?
Written by:In those with bile duct problems, and sometimes pancreatic problems, a procedure called ERCP may be recommended as a course of action. Consultant gastroenterologist Dr Gavin Johnson is an expert in the procedure, and here he explains exactly what ERCP is, and what it is used for.
Dr Gavin Johnson runs courses for trainee doctors learning ERCP in both the UK and in Europe, and leads the UK working group in setting the standards for training and competence in ERCP.
What is an ERCP?
ERCP is short for endoscopic retrograde cholangiopancreatography, but simply described, it is a procedure which is used to treat problems related to diseases of bile ducts of the liver, the gallbladder, and the pancreas.
Why is an ERCP performed?
If a patient presents with abdominal pain, jaundice, or evidence of an abdominal infection, imaging such as ultrasound, CT or MRI may show a blockage in the bile duct. The commonest cause is a gallstone that may have come out of the gallbladder, but a cancer of the bile duct or the pancreas can also obstruct the bile duct. An ERCP is the endoscopic procedure by which the bile duct, or pancreatic duct blockage is relieved.
How is an ERCP performed?
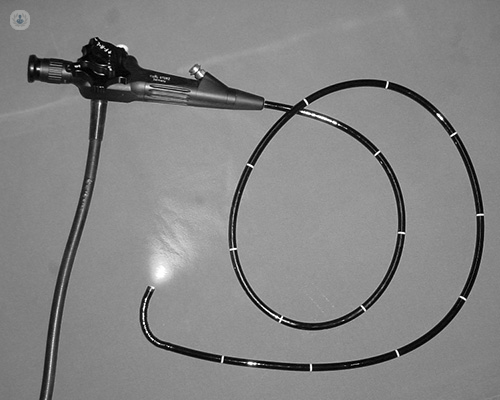
An endoscope is a flexible tube with a camera on the end of it, which is able to reach areas inside your body and give the medical professional a clear view of the internal organs or a specific area. In an ERCP, the endoscope is passed down through the mouth and into the stomach, then into the top part of the small intestine, which is called the duodenum. The bile duct and pancreatic duct open through a small nipple in this area known as the ampulla.
The doctor will then insert a very fine wire into the bile duct (or pancreas less commonly), and inject a special type of dye which shows up on an X-ray. X-rays are then taken which mean the doctor can study the bile ducts, and ducts of the pancreas. The ampulla can then be cut or stretched to allow stones to be removed, or special plastic or metal tubes, known as stents to be inserted into the duct.
Is an ERCP painful?
An ERCP is done with heavy sedation or a full anaesthetic so it is usually very well tolerated, but it can cause some discomfort during the procedure, and afterwards too. You are required to lie on your front for the procedure, and a mouthguard is used to protect your teeth.
How long is the ERCP procedure?
ERCPs usually take between fifteen minutes and an hour and a half. The average is about thirty minutes.
What can an ERCP find?
An ERCP can allow your doctor to get more accurate, detailed information about your bile duct, biliary system, or pancreatic ducts. Bile duct stones can be removed with an ERCP, along with obstructions (both non-cancerous and cancerous) and other rarer bile duct diseases.
Does the ERCP procedure have any risks?
An ERCP is widely regarded as a safe procedure but there are very important and potentially serious complications, which is why an ERCP should only ever be done with a strong indication for the need for treatment, and after the patient is made fully aware of the treatment. More serious complications include:
- pancreatitis (inflammation of the pancreas);
- bleeding, or;
- infection related to the insertion of the dye for X-rays to be taken.
Minor complications include mild abdominal discomfort and a possible sore throat. These usually disappear after a couple of days.
Do I have to stay in the hospital?
Patients can normally go home the same day of the procedure, after being monitored in the clinic or hospital for a few hours. You will know how the procedure went before you go home, but if a biopsy is taken, these results will take longer to come through.
You can resume a normal diet and general everyday activities after you leave the clinic.
If you're interested in booking an appointment with Dr Johnson, arrange an appointment via his Top Doctors profile.



