Autoimmune hepatitis
Dr Aathavan Loganayagam - Gastroenterology
Created on: 03-01-2017
Updated on: 07-27-2023
Edited by: Carlota Pano
What is autoimmune hepatitis?
Autoimmune hepatitis, sometimes abbreviated to AIH, is a chronic condition that affects the liver. As it is autoimmune, the patient's immune system attacks its own cells because the body's immune system recognises the liver cells as foreign and starts to attack them, damaging this vital organ. In the UK, autoimmune hepatitis is not common. It is estimated that around 10,000 people are living with AIH in the UK, at present.
There are two main types of autoimmune hepatitis:
- Autoimmune hepatitis type 1: It can occur at any age and is the most common. It is associated with other autoimmune disorders, such as coeliac disease, rheumatoid arthritis or ulcerative colitis.
- Autoimmune hepatitis type 2: It is more frequent in children and young people, and may be accompanied by other diseases related to the immune system.
Prognosis
If left untreated, autoimmune hepatitis can lead to scarring of the liver (cirrhosis), which can lead to liver failure.
If diagnosed and treated early on, autoimmune hepatitis can be controlled by medication that suppresses the immune system. In very extreme cases, a liver transplant may be needed when the disease is not responding to medication and it is in an advanced stage.
Autoimmune hepatitis symptoms
The intensity of symptoms can change from mild to severe and can appear suddenly. Some patients have few or no recognised symptoms and others experience them much more intensely.
Some of the symptoms of autoimmune hepatitis are:
- abdominal pain
- fatigue
- yellowish skin tone (jaundice)
- enlarged liver
- abnormal blood vessels on the skin
- skin rash
- joint pain
- absence of menstruation in women
How is autoimmune hepatitis diagnosed?
The medical tests carried out to diagnose autoimmune hepatitis include:
- Blood tests to look for antibodies to distinguish the type of hepatitis
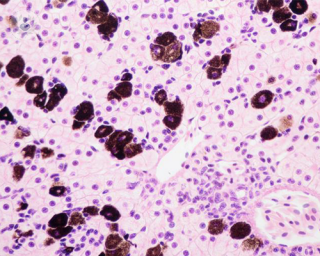
- Biopsy of the liver to confirm the diagnosis and determine the degree and type of hepatitis
- Liver function tests
- Antibody analysis
What are the causes of autoimmune hepatitis?
The main cause of autoimmune hepatitis is that the immune system does not differentiate between healthy body tissue and harmful external agents, such as bacteria, viruses and pathogens. As a result, the immune system destroys body tissues as well. It is not known why the body does this, but scientists currently believe that it could be related to environmental triggers (e.g. certain viruses or medications) and a genetic predisposition.
There are also certain risk factors for autoimmune hepatitis:
- Family history: Some evidence indicates that autoimmune hepatitis could run in families.
- Having another autoimmune disease: People with conditions such as rheumatoid arthritis, coeliac disease or Graves' disease could have a higher risk of developing autoimmune hepatitis.
- Being female: Autoimmune hepatitis is slightly more common in females.
- Infections: Certain infections are linked to autoimmune hepatitis, including measles, hepatitis A, B and C, herpes simplex, and Epstein-Barr virus.
Can autoimmune hepatitis be prevented?
Autoimmune hepatitis cannot be prevented, although diagnosing it early can help to make treatment successful.
Autoimmune hepatitis treatments
The treatment of autoimmune hepatitis aims to reduce inflammation of the liver through certain medications that suppress the immune system (immunosuppressants). By reducing inflammation, scarring can be avoided and the complications associated with this, such as liver failure. Treatment for autoimmune hepatitis is always long-term and often lifelong. In very extreme cases, a liver transplant may be needed.
Which specialist treats you?
The specialists who treat autoimmune hepatitis include hepatologists and gastroenterologists.